CHAPTER II
THE FUNCTION OF THE INTERVERTEBRAL DISC
The function of the intervertebral disc is to form a strong joint between the vertebral bodies, to allow a small range of motion between them, and to act as a shock absorber.
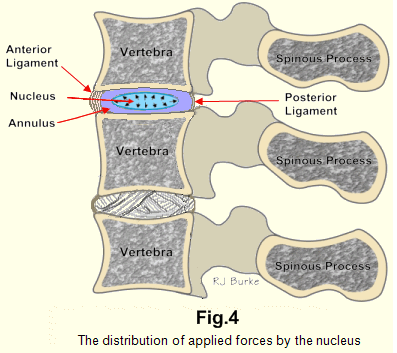
Its structure is essentially that of a golf ball, which is an almost perfect shock absorber. The nucleus (Fig.5A), a jelly, is practically incompressible. Its role is to distribute pressure equally in all directions, and so to dissipate forces exerted upon it (Fig. 4). A vivid impression of the strength of this system may be gained by placing a raw egg, which is a reasonable facsimile, in the palm of one's hand and attempting to crush it. The strongest man cannot crush it if the shell is intact. The egg feels as solid as a stone. The membrane and the shell of an egg are feeble structures compared with the great strength of the annulus supported by its peripheral ligaments and the bones above and below.
THE STRUCTURE OF THE INTERVERTEBRAL DISC
1. THE OUTER COVERING
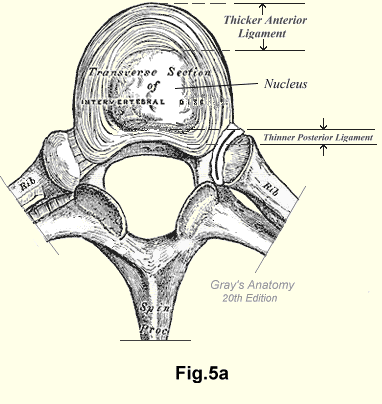
Each intervertebral disc (Fig.5A) is clothed by a tough layer of fibrous tissue, firmly attached to the vertebral bodies above and below (Fig.5B). This layer is composed of thin but quite wide bands of fibrous tissue wrapping (Fig. 5B) in various directions, so allowing a certain amount of movement between the vertebral bodies. The anterior longitudinal ligament (Fig.5A) is a strong, wide band attached to the anterior surfaces of the vertebral bodies and the intervertebral discs. It forms an integral part of the peripheral layer.
The posterior longitudinal ligament (Fig.5A) is a much thinner and weaker structure, situated within the vertebral canal. It is attached to the posterior surfaces of the vertebral bodies but is not attached to the posterior surfaces of the discs. There is no fibrous covering of that part of the intervertebral discs which forms part of the anterior wall of the vertebral canal. If there were a fibrous covering of this part of the intervertebral disc it is unlikely that herniation of the disc would ever occur. Fibrous tissue if injured, quickly heals itself. Cartilage cannot repair damage unaided.
2. THE ANNULUS
 The annulus fibrosus is composed of rings of cartilage which are
connected to each other by collagen fibrils. The space between the rings
is filled with mesenchyme. In the anterior and lateral parts of the disc
these are not concentric rings of fibrocartilage. The rings, eighteen to
twenty in number in an adult, are set at an angle to each other (Fig.5B), so that
when the disc is cut horizontally or vertically across, only a part of
each ring appears on the surface. The eight to ten posterior lamellae
which combine with the vertebral bodies to form the anterior wall of the
spinal canal run up and down, before passing forward to attach to bone.
In contrast to the rings they are parallel bands. They are firmly
anchored to bone above and below. At their lateral extremities they are
interlaced with the circumferential lamellae.
The annulus fibrosus is composed of rings of cartilage which are
connected to each other by collagen fibrils. The space between the rings
is filled with mesenchyme. In the anterior and lateral parts of the disc
these are not concentric rings of fibrocartilage. The rings, eighteen to
twenty in number in an adult, are set at an angle to each other (Fig.5B), so that
when the disc is cut horizontally or vertically across, only a part of
each ring appears on the surface. The eight to ten posterior lamellae
which combine with the vertebral bodies to form the anterior wall of the
spinal canal run up and down, before passing forward to attach to bone.
In contrast to the rings they are parallel bands. They are firmly
anchored to bone above and below. At their lateral extremities they are
interlaced with the circumferential lamellae.
The rings of cartilage are wound around the nucleus in all directions in much the same way as the rubber bands in a golf ball are wound around the liquid centre. This increases both the tensile strength and the resilience of the disc and allows a greater range of motion than would be the case if they were concentric rings. Where the rings lie in contact with bone or the cartilage plates, they are firmly anchored to these structures by fibres like Sharpey's fibres. Thus the discs form strong joints between 'the vertebral bodies which allow a small range of motion in all directions. This small range is further limited by the anterior and posterior longitudinal ligaments and by the posterior intervertebral joints.
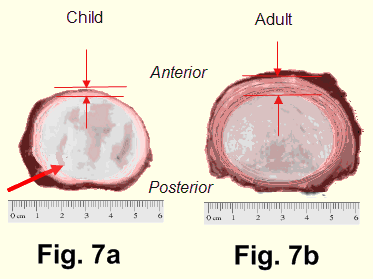
In infants the lamellae are few and indistinct. They are merely thickenings of the mesenchyme (Fig. 6 and Fig. 7a). As the child gets older the lamellae become more clearly differentiated as bands of cartilage. The lamellae increase in number at the expense of the nucleus until about the time that growth stops. The anterior and lateral lamellae are thicker than the posterior lamellae (Fig. 7b). In the adult the annulus is about twice as thick anteriorly and laterally as it is posteriorly. Hence, that part of the intervertebral disc which forms the anterior border of the vertebral canal is distinctly a weaker region. It has fewer and thinner lamellae and no fibrous covering. It can be cut or eroded easily but it has great tensile strength. The idea that a single indirect injury can rupture an intact annulus is not correct. It remains unaffected by injuries of sufficient force to cause compression fractures and fracture-dislocations of vertebrae. An injury of sufficient violence to rupture an intact annulus is unlikely to be survived by the patient.
3. THE NUCLEUS
In appearance the nucleus is a faintly greyish translucent jelly. It is mesenchyme. In the embryo the spinal column is first outlined by thickening of the mesenchyme. As the bones take shape the lamellae of the intervertebral disc begin to form and they enclose a pool of mesenchyme which becomes the nucleus of the intervertebral disc. The fact that the nucleus of each intervertebral disc is mesenchyme is the most important single factor in the etiology of backache - from occiput to coccyx - and of its radiations of Pain from head to toe.
Mesenchyme, observed Ham, typically consists of both cells and intercellular substance. Its cells possess delicate cytoplasmic arms that extend out into the intercellular substance in which they lie. The intercellular substance is an amorphous type of jelly. Mesenchyme has the latent capacity to form all the various specialized cells found in the different adult types of connective tissue.1
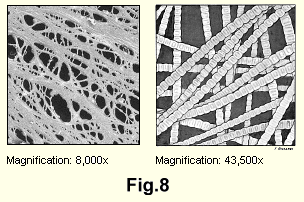
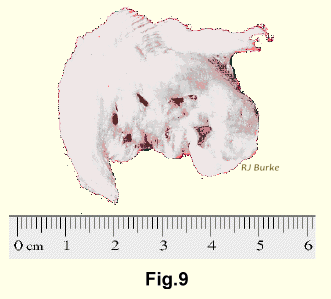
This thin jelly, if it were not restrained, would flow backward on flexion of the spine and accumulating between the posterior ends of the vertebral bodies would be capable of dislocating them. So the nucleus is restrained, its movements limited, and only small alterations in its shape permitted by the three-dimensional ubiquitous network of collagen fibrils (the cytoplasmic arms that Ham described) which are an integral part of the jelly. These collagen fibrils are attached to the inner surface of the annulus and the interstices of the network enclose the jelly (Fig. 8). In the adult the network of collagen fibres is so dense it is difficult to cut smoothly across the nucleus. When cut across, these fibrils impart a gritty sensation through the knife (Fig. 9).
It has been stated that the nucleus bulges when the disc is cut across because it has been under pressure. That is not correct because the nucleus is incompressible. All pressure can be removed from the nucleus by cutting the fibrous attachments to the bone, and still when the disc is cut across, the nucleus does not bulge. Cutting the restraining collagen fibrils releases a free pool of jelly. This pool may be elevated slightly above the surface by the elastic recoil of the lamellae.
Both the terms "annulus fibrous" and "nucleus pulposus" are inaccurate. The annulus is not fibrous, it is composed of cartilage. The nuleus is a jelly until well on in middle age when it becomes a mat of fibrillae. Pulpoisis applies only to the nucleus in old age when it has become a pulpy substance.
Mesenchyme possesses a strong inherent drive to achieve its destiny, - to become fibrous tissue, cartilage or bone; but the thick, avascular annulus, devoid even of lymph channels, protects the nucleus from all outside influences. It is susceptible only to injury.
The mesenchyme of the nucleus is able to survive for a lifetime without nourishment from the outside. The annulus is not only completely avascular; it is also, for all practical purposes, airtight. Nourishment by diffusion is not possible. The nucleus feeds on itself. As the fibrillae slowly proliferate the amorphous jelly proportionately disappears. Ehrenhaft2 has shown that its water content at birth is 88% and at the age of seventy-five falls to 69% Sylven et al have reported "The water content shows in the course of years a continuous decline."3 from birth until about the age of fifty the fibrillae proliferate until eventually the nucleus becomes almost a felt mat of fibrillae. This is the reason (and it will be explained later on) for the notable fact that after the age of fifty patients rarely suffer their first attack of backache.
The fibrillae then slowly degenerate until in old age the nucleus becomes
an amorphous greyish mass something like fine, slightly moist, greyish
sawdust (Figs.10-11).
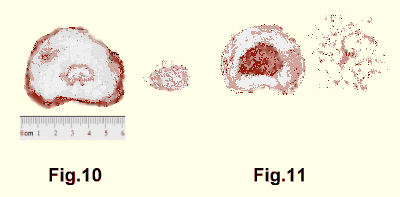 On the other hand, the nucleus that has suffered injury during life is
a pigmented fibrous mass when seen at autopsy (Fig. 12).
On the other hand, the nucleus that has suffered injury during life is
a pigmented fibrous mass when seen at autopsy (Fig. 12).

THE NERVUS SINU VERTEBRALIS
The existence of this immensely important nerve has apparently escaped recognition by the profession at large. It is not specifically described in any textbook, even those on anatomy and surgical anatomy. In two books in which it is mentioned, both the description and the illustrations are inaccurate. In these the original author is referred to as von Luschka. His name was actually Hubert Luschka. The references given are to "volume four", but the description of the nerve appears in a monograph.4
Hubert Luschka of the University of Tübingen in Germany published his monograph "Die Nerven des Menschlichen Wirbelkanales" in 1850. His account has not since been excelled and his observations have been confirmed by many European and North American investigators. A short description of the nerve he named is extracted from Luschka's monograph and given in the next paragraph, followed by a more detailed discussion.
The nervus sinu vertebralis is made up of unmyelinated pain fibres. Each nerve receives a branch from the sympathetic nervous system. It is given off by each spinal nerve from just beyond the ganglion. It returns through the intervertebral foramen. Within the spinal canal it divides into branches to the anterior surf ace of the dura, the dural sheath of the nerve root, the vessels, and to the posterior part of the intervertebral disc. Luschka was unable to find the nerve in the annulus. Since then it has been shown that on entering the annulus it breaks up into a great number of micro-scopically fine branches which end in minute terminal nodes.
The above short description fits the clinical picture well but some notice must be taken of the great amount of study that has been done by many men on these nerves. The tracing of these little threads is one of the most difficult problems in anatomy. We have attempted to trace it in the gross more than twenty times and have ended in frustration. On one occasion we had the unusual opportunity of examining a spine about two hours after the death of a thirty-year-old man in a traffic accident. We followed the nerve, we thought, quite successfully. It was traced from the anterior surf ace of the dura and the posterior surface of the disc to the intervertebral foramen and to the spinal nerve. Photographs of the nerve proved to be failures, and microscopic sections were not found to be convincing to our pathologists.
About ten years ago in more than fifty cases of routine autopsy we removed portions of the posterior annulus from the vertebral canals. We sectioned and stained them in many ways, but were unable to convince the pathologists, or for that matter ourselves, that here indeed were unmyelinated nerve fibres. By superimposing sections we attempted to obtain a recognizable pattern, but this too was a failure. Our position was the scientifically correct one of doubt. We wondered if unmyelinated pain-transmitting fibres really existed. We questioned whether anyone actually had demonstrated them, and whether pain might be transmitted by some mechanism in physical chemistry that is at present entirely unknown and unsuspected by us. These doubts have been resolved by the work of many researchers who have convincingly demonstrated the presence of the nervi sinu vertebrales.
As a result of our own explorations we acquired a profound respect for the meticulous and detailed investigations of Luschka. He wrote that many times he had followed a little thread which penetrated the intervertebral disc, and "no doubt entered the bone from there" since he could not discover the nerve inside the disc in spite of repeated examinations of its tissue (Fig. 13).
ANATOMICAL NOTES
Many investigators, most of whom were aware of Luschka's work have reported on parts or the whole of this nerve, whose sole reason for existence seems to be to add to the sum of human misery - a purpose that it accomplishes admirably!
Of those who followed or attempted to follow the gross anatomy of the nerve, almost all commented on the extraordinary difficulties of the procedure.
Armstrong5 and Bradford and Spurling6 mention the existence of this nerve, and the 1959 edition of Gray's Anatomy notes that "a small meningeal branch is given off from each spinal nerve after it emerges from the intervertebral foramen. This branch re-enters the vertebral canal through the foramen, supplies afferent fibres to the vertebrae and their ligaments and carries sympathetic postganglionic fibres to the blood vessels of the spinal cord and its membranes".7
Jung and Brunschwig8 demonstrated unmyelinated nerve fibres in the posterior longitudinal ligament, but found none in the discs themselves. Kaplan9 observed that a branch of the nervus sinu vertebralis breaks into fine filaments which are distributed over the anterior surface of the dura.
Wiberg10 dissected out the nerve and noted that the dissection was particularly difficult and that this was probably the reason for the different findings of different workers. He too observed that it was joined by a branch of the sympathetic, but he was unable to find any nerve fibres in the annulus.
Hovelacque11 supported Luschka's view that the nervus sinu vertebralis is formed by a branch of each cerebro-spinal nerve joined by a branch from the sympathetic, so that a single stem passes through the intervertebral foramen. Hovelacque followed the nerve and found that it divided into branches which ended in fine fibres in the dura, the outer surfaces of the vertebral bodies, the ligaments and the vessels.
Pederson et all12 reported a remarkable study in which they followed these nerves throughout their courses by serial microscopic sections. They followed the nerves bilaterally, as they branched from the spinal nerves just distal to the ganglia. They observed that the filaments were so small that the sections had to be studied repeatedly in order to trace their distribution accurately. They traced nerve fibres to the dura mater and to the margin of the annulus fibrosus. They did not find fibres within the annulus.
Roofe13 found recurrent branches of the spinal nerves returning from beyond the dorsal root ganglia to the vertebral canal through the intervertebral foramen. He observed many unmyelinated nerve fibres in the tissue of the annulus fibrosus which, he stated, terminated in nerve endings within the annulus. From consideration of the microphotographs shown by Roofe we judged that he followed the nerve for a distance of 0.05 mm into the annulus and then lost it as it broke up into its terminal branches.
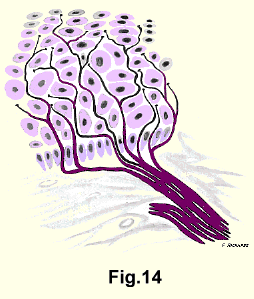
Ham14 theorized that the element or unit - of the receptive mechanism for pain is not a small encapsulated structure innervated by a nerve fibre, but rather an appreciable area over which the naked unmyelinated terminal branches of each neuron are distributed. These naked fibres branch freely and end in fine beaded terminals (Fig. 14).
It would be more accurate to say, since these are afferent nerves, that they arise in the annulus, the dura and the dural sheaths of the nerve roots, and pass through the intervertebral foramina to the spinal nerves.
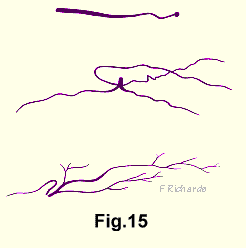
Malinsky15 published excellent microphotographs of the origins of the nervus sinu vertebralis in the annulus. He stated that an essential condition for good demonstration of the nerve fibres is correct fixation. He said that the interval between the patient's death and the fixation of the material must be as short as possible, from two to six hours.
Malinsky made drawings from these microphotographs, three of which are here reproduced with permission (Fig. 15).
SURGICAL NOTES
Many surgeons have recorded their impressions of the sensitiveness of the intra spinal structures as the result of specific investigations, and of intervertebral disc operations under local anaesthetics.
Hirsch performed transdural puncture under x-ray control of the affected intervertebral disc in sixteen cases of backache, "all of which had been resistant to prolonged conservative treatment." He observed that pain occurred at the moment of puncture of the posterior annulus, and on moving the needle up and down in the substance of the annulus. By injecting normal saline into the nuclear space and increasing the pressure, he produced pain identical with the patient's spontaneous pain, i.e. lumbago and sciatica.
It seems clear that Hirsch's experiments demonstrated that the posterior annulus was sensitive to pain on its posterior surface, in its substance, and on its inner surface.
In another report Hirsch wrote that in a degenerated disc up to 2cc of normal saline could be injected. If the pressure were raised during the injection, the patient suffered severe pain of a type which he could clearly identify as the pain he was accustomed to during an attack of "lumbago-sciatica". The addition of local anaesthetic soon relieved the pain, which reaffirmed that pain can arise from the inside surface of the annulus. He also noted that the severity of the pain was proportionate to the pressure applied by the plunger of the syringe to the internal surface of the disc17.
Lindblom and Perey18 reproduced both backache and sciatica by injecting affected nuclei with contrast media under pressure. They relieved the pain by injecting a local anaesthetic solution.
Wiberg19 operated on two hundred cases after inducing local anaesthesia down to the ligamentum flavum. He reported that touching the disc itself caused pain in the lumbo-sacral distribution in nearly all cases, and the patient stated that he felt as if the pain were inside the back. Wiberg thought that palpation of the root caused root pain. He observed that after anaesthetizing the root the patient still felt pain in the leg, and he wondered if, in this case, the recurrent branch of the nervus sinu vertebralis from the opposite side transmitted the pain. He also found that touching the vertebral bodies inside the vertebral canal did not cause any pain.
Falconer20 found in operations under local anaesthesia that light pressure on the affected annulus reproduced the backache, but not the sciatica. He did not regard pressure on the root in its intrathecal course of importance, because the nerve is loose and easily slips away from pressure in this area, unless the tumour be large enough to occlude the thecal lumen completely.
Cloward21 (1959) confirmed the findings of the Swedish orthopaedic surgeons but in the cervical spine. In the performance of cervical discography he injected solutions into the affected cervical intervertebral discs and found that this reproduced or exacerbated the pains from which the patients had previously been suffering.
We quailed at the prospect of driving a needle transdurally into a nuclear space in a fully-conscious patient. Our reluctance was increased by the conviction that if, by mistake, a normal nucleus were penetrated, another intervertebral disc lesion would be started.
We confirmed the surgical observations made with the limited local anaesthesia described above although in only two cases. Operation under general anaesthesia is so much easier on the patient and on the surgeon, that that was enough. It appeared to us that mild irritation of the dural sleeve, or of the anterior surface of the dura, or of the posterior surface of the annulus caused backache. The abrasive action of cutting a hole in the posterior annulus with a curette caused a great increase in the backache plus sciatic radiation. The patients identified these pains as the ones from which they had previously suffered.
BLOOD SUPPLY
Neither the annulus nor the nucleus has any blood supply at any time of a person's life.