CHAPTER III
THE ANATOMY OF PAIN IN BACKACHE
THE TWO KEYS
1. The first key to the problem of backache is the predictable change of the mesenchyme of the nucleus to fibrous tissue - the result of rupture of fibrillae in the nucleus. The first attack of spinal pain arises from the intense pressure of the small free pool of mesenchyme thus released on the sensitive posterior wall of the annulus. Subsequent attacks are the result of pressure and erosion by the fibrous nucleus on the same surface. Therefore "nuclear lesion of an intervertebral disc" is a diagnosis based on etiology. Examinations of surgically excised abnormal nuclei show them to be composed largely of fibrous tissue and also to contain fibrocartilage and cartilage in varying, and much smaller, amounts. For the sake of brevity the abnormal nucleus will hereafter be referred to as the "fibrous nucleus".
2. The second key is provided by the nervi sinu vertebrales which arise in pairs from the posterior part of each annulus, the anterior surface of the neighbouring dura and the dural investments of the nerve roots. They transmit the pain, and in transmitting they induce the radiating pain.
THE RUPTURE OF FIBRILLAE AND THE CHANGE TO FIBROUS TISSUE
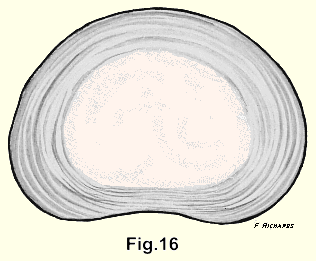
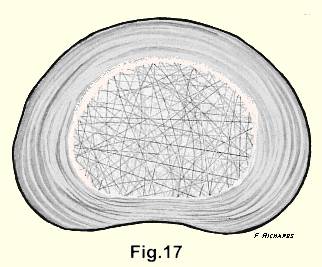
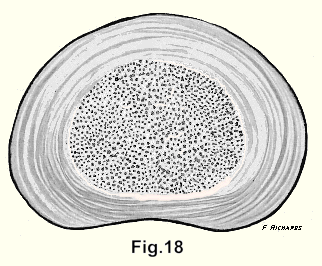
The spinal column is formed from mesenchyme, and as it develops, each cartilaginOus annulus encloses a pool of mesenchyme which becomes the nucleus of the intervertebral disc. The thick avascular airtight annulus protects the nucleus from- all outside influences. It is vulnerable only to injury and to the slow change that occurs with aging (Fig. 16, 17, 18).
The patient who has suffered his first attack of back pain may remember, for example, that he bent forward and twisted his spine to pick up an object from the floor. He felt something snap, or tear, or "go out of place" in his back, and this was followed immediately or after an interval, by pain. Some patients fall to connect the commonplace motion with the attack of pain, while others, if some time has elapsed, may have forgotten the incident.
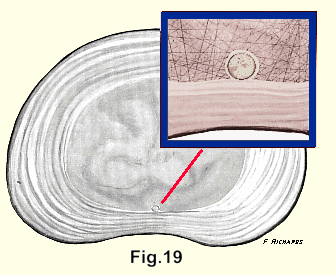
Flexion of the spine places the collagen fibrils in the posterior part of the nucleus under tension and rotation of the spine in the flexed position applies the powerful force of torsion to the fibrils and may snap them. The accident releases a small pool of jelly which is subjected to the same pressure as the whole mass of the nucleus (Fig. 19). The nucleus is now made up of two pools, one large pool, and one small pool close to the posterior annulus. The much greater pressure exerted by the small pool on the inner surface of the annulus is examined further on.
It is probable that the injury to the nucleus is not only physical but chemical. The jelly and the fibrillae are parts of the same molecular structure and the' injury breaks the molecular chain. The injury starts the nuclear jelly on the way to transformation into fibrous tissue and it seems that once the change is started, it proceeds rapidly until the whole nucleus has been converted. At operations and at autopsies, at least, we have never observed a nucleus which was partly jelly and partly fibrous tissue.
The pool of jelly which is originally released may be so minute that it is not perceived by the terminal beads of the nervus sinu vertebralis; but the fibrillae surrounding this small pool are driven from their normal course. They are stretched, and further move ments of the spine snap them until a pool sufficiently large to irritate the nerve endings is formed. This accounts for the delayed onset of pain in some of these cases, for hours or even for a few days. An example is the patient who reports that as he picked up a piece of paper off the floor of the factory two days ago, he felt something snap in his back but it did not bother him much. He continued working but this morning he was unable to get out of bed because of the severe pain in his back. His insurance claim is likely to be rejected on two counts.
1. The accident should have been reported at once.
2. Such a slight accident can hardly be regarded (by any rational examiner) as the cause of such excruciating pain, especially after a two-day interval.
Therefore insurance companies and compensation boards take the firm and apparently reasonable stand that the trifling back injury must heal up in a few days. If pain and disability continue, or recur and recur, year af ter year - as they will if improperly treated - the companies are likely to conclude that the patient is either malingering or neurotic. This causes a sore point between doctors and their patients on the one hand and insurance companies on the other, which seems to be universal. In Sweden Professor Carl Hirsch wrote that "insurance companies cannot understand why such severe and prolonged disability can follow such a minor injury1.
In order to demonstrate that rupture of fibrillae in the posterior nucleus is the primary cause of back pain it would be necessary to cut fibrillae by thrusting a knife - or a needle - through the annulus into the nucleus. It would have to be done in human subjects because the patient's report is of almost total importance in these lesions. This experiment has been done for us by the accidental insertion of spinal puncture and myelogram needles into nuclei and the results have been published in many articles in the literature2,3,4,5,6,7. Where histories are given by the authors, they are those of nuclear lesions of intervertebral discs. Some authors suggested, that the path of the needle might pave the way for herniation of the nucleus. But a needle passed through only one lamella results in a self-sealing puncture. It is quite improbable that if eight or ten lamellae were punctured, the jelly could ooze through that number of layers, and find its way into the spinal canal. The fact that the lamellae are separated from each other by mesenchyme- filled spaces makes such an excursion a physical impossibility. Such patients require the same treatment as all other patients who have nuclear lesions. We have had a few of them who eventually came to surgery. None had progressed to herniation of the nucleus. The nuclei showed the same changes, both gross and microscopic, as in all other disc lesions. The normal jelly had long since become fibrous tissue, and it was observed at operation that the posterior annulus in each case was quite thin. It had been extensively eroded on its inner surface.
In these cases there can be no doubt that the injury by the spinal puncture needle caused the change of the nucleus from mesenchyme to fibrous tissue plus varying amounts of fibrocartilage and cartilage, and it seems certain that the stimulus is the result of cutting fibrillae. The number of fibrillae that would be cut can only be wondered at, if one compares a spinal needle with the drawing made from Bengt Sylven's electron microphotograph (refer to Fig. 8). This picture is reproduced to scale, and the magnification is 43,500 times. If the needle had punctured the nucleus to a depth of only one-quarter of an inch, it would have penetrated and cut fibrillae on the same scale as this to a depth of one thousand feet, and the diameter of the needle would be about two hundred and fifty feet.
Many times in routine autopsies on children and young adults, we have removed sections of the spine, each of which included three intact intervertebral discs. After observing that the nucleus of the intervertebral disc below the segment and that of the nucleus of the intervertebral disc above the segment, both presented a normal jelly-like appearance, we presumed with almost total justification, that the three intervening nuclei presented the same normal appearance. Then, using as aseptic a technique as was possible under the circumstances, we drove a spinal puncture needle through the annulus into the nucleus in each of the three intervening discs. The specimens were kept at room temperature and after waiting about four weeks we found on cutting the discs horizontally that in every case the jelly had moved up on the evolutionary scale. A typical report is that of pathologist Campbell F. Coady who wrote, "Multiple sections failed to demonstrate the usual normal nucleus pulposus, and histological sections demonstrated fibrous tissue and fibrocartilage only."
It seemed reasonable that if we were to cut intervertebral discs horizontally so that maximum injury was inflicted on the fibrillae and place them in normal saline, a fine crop of connective tissues would grow. What happened was that the nucleus, in a few hours, began to swell. After one day its appearance did not change (Fig. 20). The jelly seemed to be thinner and more watery than normal. What happened was that the mucopolysaccharides of the nucleus had absorbed the normal saline, and after three weeks, microscopic sections further showed, as reported by pathologist P. S. Vassar: "severe post-mortem autolysis with heavy bacterial contamination. Presumably massive digestion of tissues has occured as a result of proteolitic enzyme activity released by necrotic cells and bacteria".

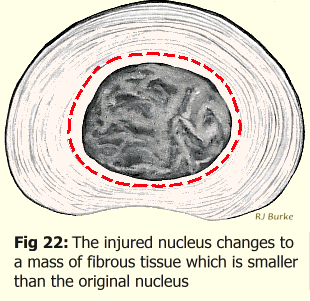
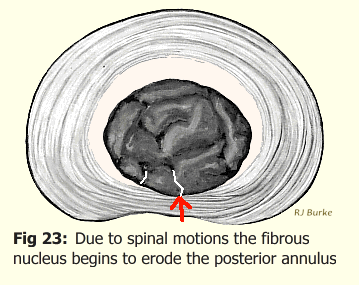
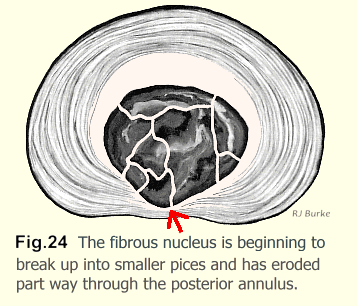
It is probable that, following the rupture of fibrillae and the consequent stimulus to the mesenchyme in the living patient, the change of the whole nucleus from jelly to a firm fibrous mass takes about three weeks. It is notable that in many of these cases the pain abates slowly over this period. The fibrous nucleus is about 2cc smaller than the original volume of the mesenchyme, so it tends to retract from the annulus. Thereafter, because of spinal movements, pain tends to recur and recur, sometimes with little relief between exacerbations. Almost all movements of the spine are flexion, plus rotation coupled with lateral flexion, and the recovery from these positions to the upright position. Flexion drives this firm fibrous mass back onto the posterior annulus, and rotation imparts movements to the fibrous mass, which slowly and painfilly erode the softer annulis.
Normally, from infancy on the fibrillae increase in number at the expense of the jelly until, after the age of fifty, the nucleus resembles a moist felt mat more than it does a jelly. This mat is incapable of exerting any particular peripheral pressure on the inner surface of the annulus. The felt-like mat is resistant to rupture of fibrillae. The mesenchymal jelly has now been replaced by fibrillae so that even if some fibrillae were ruptured the nucleus would not be capable of changing to fibrous tissue. That is why the first attack of backache due to a nuclear lesion almost never occurs after the age of fifty. Hirsch8, Hult9 and Lundgren10 who between them exhaustively examined more than twenty-thousand patients with backache found that the oldest patient suffering from his first attack of backache in any part of the spine, was forty-nine years.
Ultimately, some time after the age of fifty the mat becomes broken up and disintegrated due to lack of nourishment and the constant grinding by the opposing vertebral bodies.
If the nucleus has been injured and has changed to fibrous tissue the fibrous tissue also is unable to get nourishment. It too, very slowly becomes broken up and disintegrated. Sometime after the age of fifty it becomes an amorphous substance. It is pigmented because the fibrous nucleus is pigmented, but otherwise the end result is much the same. It is at this stage that pain from the injured intervertebral disc ceases.
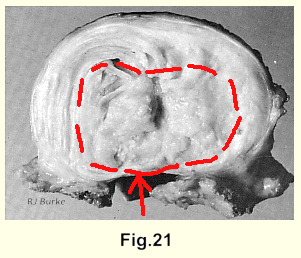
If the fibrous nucleus has eroded through the annulus and has contacted blood supply in the spinal canal it persists as fibrous tissue indefinitely (Fig. 21), although in a very few cases it becomes converted to bone.
We know too, from surgical experience, that in young and middle-aged people the change from mesenchyme to fibrous tissue as a result of injury to fibrillae always occurs and that it is easy to locate the exact level of the lesion (the site of irritation) by the simplest of clinical means (page 95). In cases with relatively short histories the nucleus has changed to a large mass of fibrous tissue which is easily identifiable as such, after excision, both grossly and microscopically. In the cases with long histories the fibrous mass has become fragmented (Fig. 22, 23, 24).
It is rarely that one has to operate on a patient within the first few years after the onset of a backache. It takes a long time for the fibrous nucleus to erode into the posterior annulus to the point where it cannot be dislodged by manipulations of the spine. These patients remember, often only after some effort and time, that it was fifteen or twenty years or more ago that they suffered their first attack of backache of the same type. It it a mistake to date the onset from the beginning of the last acute exacerbation.
The following is a pathologist's report on an excised nucleus:
"Sections through various portions of the tissue show fibrous tissue with some fibrocartilaginous tissue and degenerated hyaline cartilage. There are marked degenerative changes with the matrix being homogeneous and somewhat eosinophilic in character. The areas of degenerating fibrous tissue and fibrocartilage merge imperceptibly with a structureless, somewhat fibrillary, relatively acellular, slightly eosinophilic material showing within its substance occasional pale cells with pycnotic nuclei.
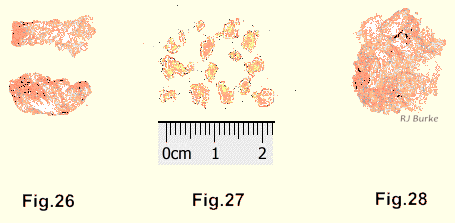
Such a report does not describe an unknown and mysterious tissue - it is a fibrous tissue that has been starved and injured over a long period of time. After many years of presenting these specimens to our pathologists and discussing the subject with them, we find that our reports now simply state "fibrous nucleus of an intervertebral disc" (Fig. 26, 27, 28, 29).
The nuclear lesion is unique because neither the annulus nor the nucleus of the intervertebral disc has a blood supply. A profound change occurs and a great variety of pains follow without any of the reactions of inflammation, and no attempt at healing can be made. That is, not until the posterior annulus is worn through. At this point blood supply may be contacted and an attempt made to patch the defect with fibrous tissue.
When the disc loses its efficiency as a shock absorber the bone of the vertebral bodies, above and below, begins to grow outward and around the disc to support it and to limit further the normally small range of motion. It occasionally proceeds to fusion between the bodies. It has been described as exostosis formation which, in a sense, it is, although an exostosis is usually a nuisance without any helpful function. It is also described as osteoarthritis of the spine, which, most certainly it is not.
In children and old people backache presents a somewhat different, much less frequent and usually an even simpler problem. In children the fibrillae are comparatively few in number and are quite loose. In old people the nucleus has become an amorphous substance. In each of these cases it seems that the nucleus, through various motions of the spine, becomes pushed to the posterior end of the nuclear space and the accumulation there causes an increased pressure on the annulus which creates discomfort rather than the severe pain often seen in the middle-aged victims. Fortunately these two groups are amenable to treatment by manipulation of the spine and almost always their recovery is secured with one or two treatments. If the pain recurs another treatment or two will relieve it again. If the patient is not promptly relieved the diagnosis must be reviewed. It is mostly in the young and the old that the exceptional causes of backache occur.
Very, very rarely in young children the nucleus changes to fibrous tissue and wears through the annulus into the spinal canal. King11 reported confirming the diagnosis of a herniated disc in a three year old at operation.
THE REMISSIONS OF PAIN
The spontaneous remissions of pain in these lesions are accounted for thus:
1. A movement of the spine thrusts the fibrous mass forward and away from the sensitive area, and,
2. As erosion continues, one lamella is worn through and there is a pause before pressure and erosion are exerted on the next layer. Therefore, following a period of incomplete relief exacerbations are to be expected.
The deliberate remissions of pain are secured by traction and manipulation of the spine, and, in the comparatively few cases in which this fails, by excision of the fibrous nucleus, preferably before it herniates into the spinal canal.
THE FORCES ACTING ON THE INTERVERTEBRAL DISC
A calculation that has had considerable circulation and credence among medical men concerns a man lifting 100 pounds (45kg) in weight. It was assumed that the lever of the spine was 75 cm in front of the fulcrum of the lumbo-sacral disc, and 5 cm behind it. The mechanical advantage then is 15: 1. It was estimated that the moment of force of the 100 pound weight is 1500 pounds which must be balanced by the erector spinae muscles. The muscles must pull with a force of 1500 pounds which exerts a total force of 1600 pounds on the lumbo-sacral disc. It was noted that even this figure ignored the moment of force of the head, shoulders and trunk which were in front of the fulcrum and which must be balanced by muscular effort.
This calculation is the basis for a Workmen's Compensation Board rule that a man must get help in lifting weights over100 pounds. The calculation is incorrect and the rule is not related to reality.
The nuclear injury is suffered as the result of a free, vigorous and unguarded motion of the spine. A man about to lift a heavy weight braces himself and does most of the lifting with his legs. Two long levers are involved, the spine and the legs, joined by the hip joints. Many weight lifters are able to lift 400 pounds from the floor over their heads. While doing so they flex their knees and hips and maintain their lumbar spines in extension. The lift, according to the above calculation, would apply a minimum weight of 6400 pounds on the vertebral bodies. This is about the weight of a large car plus a small car. It would crush the vertebral bodies.
Another quite popular medical calculation, which attempts to explain low back pain concerns a man whose spine, from the sacrum to the base of the neck, is 2 5 inches long. His arms are 2 5 inches long. His lumbo-sacral disc is 1/2 inch deep. The mechanical advantage is 5 0 inches to 1/2 inch or 100-to-1. If the man bends forward with his arms outstretched to lif t a 10 pound bag the pressure on his lumbo-sacral disc is 1000 pounds! Each lumbar vertebra takes the full weight applied to each vertebral body above it, plus the weight of the body intervening. So in this case the weight-lifter's 5th lumbar body would be supporting 40,000 pounds plus the weight of his body above the 5th lumbar vertebra! The sudden application of such a force might reduce a vertebral body to its constituent atoms.
We have had many discussions on the forces affecting an intervertebral disc with the engineers, physicists and mathematicians of the Research Council at the University of British Columbia. Mr.R. W. Klinck (Head of the Department of Engineering) and engineer Dr. Levelton even attended autopsies in which sections of spines were removed and the structure and movements thereof were observed. They constructed a simple working model of a section of spine for more leisurely contemplation.
The problem was to keep the mathematical considerations simple enough to be understood by the author and other doctors and yet maintain validity. The result of our deliberations was that Mr. Klinck wrote the following:
"I must confirm my misgivings about setting up a general equation to cover the mechanics of applying compressive and shear forces to an intervertebral disc. The sharing of load by the tension elements of the mechanism appears to introduce complications serious enough to make it difficult to set up either a mathematical formula or an elaborate experimental model which would yield useful results.
"Since you have insisted on 'simplicity' I have taken the requirement literally and set out the simple mechanics involved in applying compressive or shear forces to the disc.
"After the amount of thinking I have enjoyed doing on this problem I am appalled at the paucity of the technical results."
Klinck proceeded:
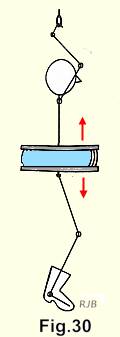
"Consider a hypothetical body whose principal attributes are weightless strength and an unusual ability to keep one intervertebral disc horizontal. For purposes of calculation let us assume that this disc is 1Y8 inches in diameter, in consequence of which it has a plan area of 2 square inches. When this body hangs by his arms from an overhead bar (Fig. 30) the tissues surrounding the spine support the whole weight of his boots, because the disc cannot sustain a tensile load. Thus, such loads place the disc in no jeopardy.
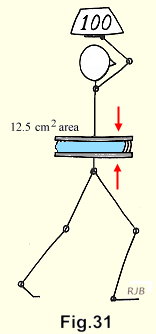
"When the body goes in for weight lifting (Fig. 31) he is wise enough to hold the 200 lb. one directly above his disc. This gives a uniform compressive load of 200/2 = 100 pounds per square inch on the disc, a value which is a useful basis for comparison with a value to follow.
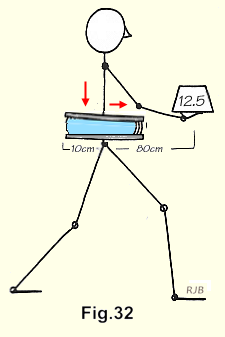
"When the body settles for one-eighth the weight (25 pounds) and carries it as in Figure 32, he actually increases the compressive load on his disc because his spine is now in both compression and bending. To support the bending moment of the weight about the disc, the muscles of the back must develop a force of 24/3 x 25 = 200 pounds. The disc must support this force plus the weight itself, i.e. 200 pounds plus 25 = 225 pounds, so that the compressive load on the disc is now 112 pounds per square inch, or 12% more than for an overhead weight of 200 pounds.
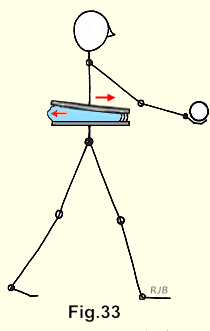
If the 25 pound weight in Figure 33 is replaced by a horizontal force perpendicular to the paper the body might be catching a ball, as in Figure 33. This applies another type of load to the disc, known as a shear load. In this case the top of the disc will tend to slide horizontally past the bottom, both in translation and rotation.
"The body's activities serve to illustrate the mechanics which induce compressive and shear forces on a disc; and to suggest the complications invoked by a human body endowed with weight as it engages in a combination of activities in a variety of attitudes."12
THE MATHEMATICS OF THE RELEVANT INTERNAL FORCES IN THE DISC
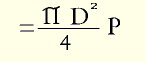
The nucleus of an intervertebral disc is approximately a circle in horizontal section. It is an ellipse in vertical section. The computations involved in estimating the forces applied by such a figure are complex. However, it is valid, for our purpose, to regard the nucleus (Fig. 34) as a sphere, and also to regard the small free drop of jelly as a small sphere (Fig. 35).
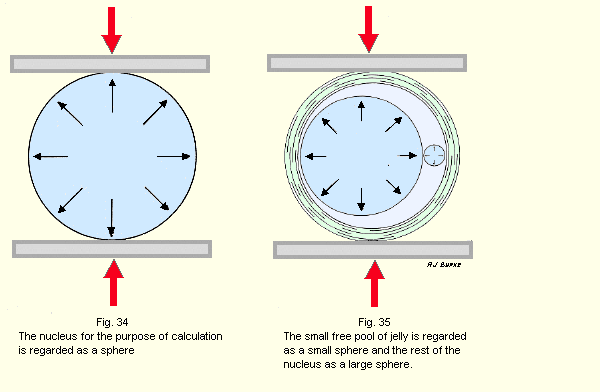
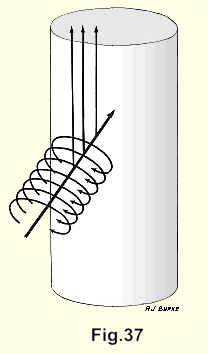
Then: The pressures exerted by the two spheres:
If
W = weight on vertebral body
D = diameter of the larger sphere
d = diameter of the smaller sphere
P = pressure exerted in pounds per square inch
The pressure in the large sphere may be regarded as the same as in the nucleus:
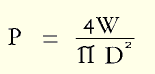
The radial force on the small sphere:
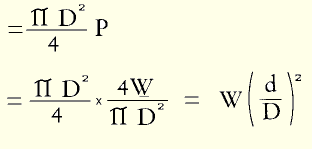
The pressure inside the small sphere is also P.
While very small the little sphere, with great pressure exerted equally on all areas of its circumference, acts as a solid. It bears on the inner surf ace of the annulus over a diameter g and pressure P per unit of surface area on the annulus is given by:
To this figure must be added the radial pressure exerted by the large sphere on the small sphere.
The small sphere behaves much like mercury which has been dropped on a clean glass surface. The minute drops are spherical. The larger volumes lie in flat pools.
SUMMARY
The small sphere exerts great pressure on a very small surface of the annulus. As it enlarges and flattens the pressure rapidly decreases,
THE TRANSMISSION OF PAIN
The posterior annulus (i.e. that part which forms a border of the vertebral canal) is sensitive to pain on its posterior surf ace, in its substance, and on its inner surface. The anterior surf ace of the dura and the dural investments of the nerve root are pain-sensitive.
Pain sensations are transmitted by branches of the nervus sinu vertebralis, one from each side, which originate in the posterior part of each annulus and in the anterior surf ace of the dura, and the dural sleeves of the nerve roots. These are aching pains.
Pressure on a nerve root by a herniated disc (or anything else) causes painless motor and sensory paralysis attributable to that root. In doing operations under local anaesthesia, retraction (or movement, or mild compression with forceps) of nerves may cause a momentary "electric -shock- like" stab of pain or a twitch of muscle but continued steady retraction does not cause a continuing pain. It is probable that a pull on a nerve stimulates either the nerve cells, the nerve endings or both and that a mild blow on a nerve, for example, being struck on the u1nar nerve at the elbow, creates a similar effect. The same "momentary electric-shock-like pains" occur in doing myelograms if the needle pushes a nerve aside or thrusts it ahead.
A THEORY OF THE RADIATION OF PAIN
The radiating pain resulting from nuclear lesions differs from referred pain. A classical example of referred pain is that of the irritation of the diaphragm as the result of rupture of the spleen. Pain is referred to the skin over the top of the left shoulder. Both areas are supplied by C 3-4. In contrast to this is the fact that the "pseudo-sciatic" radiation of pain in a low lumber intervertebral disc lesion cannot be attributed to any particular nerve root or possible combination of nerve roots. Consider for example the common radiation which runs from the lower lumbar region into a buttock and all the way down into the toes.
The functions of nerves depend on the flow of electrical current and although one cannot be sure how close a parallel there is between an electrical system built by an engineer and the network of nerves in the living body, some deductions may be attempted.
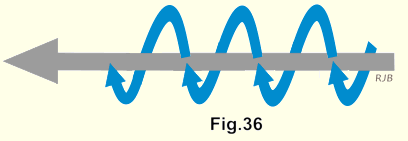
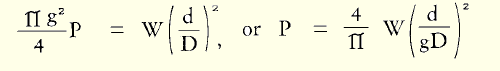
An electric current running along a wire sets up a magnetic field about it, and the stronger the current the stronger the field. If the current varies (as it does in the nuclear lesion, since slight spinal movement is constant) the magnetic field changes in density which will induce currents in circuits lying in the magnetic field. The electric currents run in the opposite direction to the original current (Fig.36).
We know that after the mesenchyme of the nucleus has been converted to fibrous tissue, erosion of the annulus begins as a result of spinal movements. At first there is only spinal pain but later the radiating pains into the limbs, the head, or the wall of the trunk begin. As erosion continues a greater number of the minute terminal nodes of the nervus sinu vertebralis are contacted, and a greater electrical current is stimulated, which runs along the unmyelinated (non-insulated) thread of the nervus sinu vertebralis.
Thus it may be that a strong and varying current resulting from stimulation of a great number of the terminal nodes of a nervus sinu vertebralis would similarly cause a magnetic field around it. Electrical currents would be stimulated to flow in the opposite direction, i.e. in the direction of the brain, along the circuits provided by receptive afferent tracts. It is probable that the most receptive are the unmyelinated pain fibres associated with the spinal nerves in the spinal cord. These currents would then be interpreted by the cerebral cortex as a variety of sensations, mostly painful, from the limbs or elsewhere in the distribution of the spinal nerves (Fig.37).
The result is the same as that in referred pain. The sensations are falsely projected to a region remote from - the area stimulated. The f alse reference is due to central misrepresentation in each case. The confused reference of the stimuli accounts not only for the pain that the patient suffers but also for the difficulties of the examiner. To the patient the pain in the limbs, the head or in the wall of the trunk is real and may be totally disabling; but the examiner who searches the limbs and elsewhere for signs is able to find nothing. This leads to a great number of these patients being labeled, quite unfairly, as malingerers or neurotics.
The issue is further clouded by the f act that a doctor's thinking is rooted in the reactions of inflammation. His examinations are largely based on searching for the signs of inflammation. In nuclear lesions of intervertebral discs there is no inflammation because the annulus has no blood supply. The lack of physical findings is a notable feature of the nuclear lesions of intervertebral discs.
AN ASIDE ON ELECTRICAL INVESTIGATIONS
A great deal of investigation has been done into electrical phenomena in living bodies, much by medical men but also a great deal by electrical engineers. A few examples follow.
Becker13 has shown that association of the DC bioelectric field with central nervous system elements demonstrated the longitudinal flow of charge carriers within that system. Transverse DC Voltage, attributed to the Hall effect, has been obtained from the extremities of intact salamanders under circumstances indicating electric currents. These voltages disappeared af ter nerve section.
Electrical engineers have done and continue to do remarkable work on cardiac arrest and cardiac resuscitation.
Uretz14 has described in detail the eye of the frog as the model for electronic devices and systems.
Norris15 has measured the electrical activity inside single muscle cells. He has observed peculiar voltage oscillations in the muscles of a patient with myotonia.
Brosnan16 notes that "a magnetic field changes the rotational speed of cell plasma, the rate of growth in plants and the agglutination of chromosomes and even that it alters tissue structure. "It has aptly been confirmed by experiment that the human body (as a whole) produces or can produce its own electric and magnetic field."
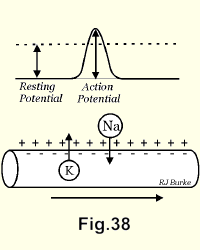
Katz17 illustrated the action potential travelling (in direction of arrow) along the axon. During the rise of the wave, sodium ions enter the fibre and charge the interior positively. During the decline, potassium ions leave the fibre and restore the initial membrane potential (Fig. 38).
Observations have also been made on the production of acetylcholine at some nerve endings. We wonder if this and the movement of ions is not an effect of electrical current flowing in living tissues rather than a cause of anything significant.
A doctor who had visited Russia and who was aware of my interest in tantalum18 told me that a Russian scientist had, in animals, removed sections of the sciatic nerve and had interposed tantalum between the cut ends. The animals walked around without evidence of disability for a time, probably until the nerve ends became covered with fibrous tissue. If the report were only partly true the experiment would be a good demonstration of the fact that nerves are simply transmitters of electric current between end organs and the brain. The report is in need of confirmation but I have been unable to get any further information. However, it is unlikely that the cut ends of the nerve could be placed so exactly opposite each other that electric currents would pass both ways along the proper channels via the intervening metal.
MUSCLE SPASM
Much of the pain in backache has been attributed to muscle spasm and a great deal of therapeutic effort has been directed at the relaxation of muscles. In an acute case in the cervical spine paraspinal muscle spasm is evident. If there is radiation to the shoulder and down the arm, the doctor can of ten feel spasm of the supraspinatus the deltoid and the extensor muscles of the forearm.
In an acute lumbar lesion paraspinal muscle spasm of almost board-like rigidity is of ten present from the top of the sacrum up to the level of the middle of the scapulae. If there is radiation of pain into the legs from a lumbar disc lesion there may be palpable spasm of the gluteal, the hamstrings and the calf muscles.
Muscle spasm is always present in cases of nuclear lesions even if it cannot be palpated. In 1934 Wedell and Finestein19 reported that if the muscle spasm were not clinically demonstrable in backache it could always be shown to be present by electromyographic investigation. They demonstrated the constant increased irritability of the local muscles indicating continuous involuntary spasm. They concluded that the spasm was not induced by involvement of the nerve root, but by a secondary source of pain, the origin of which, they said "is obviously unknown".
PROTECTIVE MUSCLE SPASM IS NOT PAINFUL
A classic example of protective muscle spasm is the board-like rigidity of the abdominal muscles in the case of perforation of a peptic ulcer. The pain is inside the abdomen. It is not in the muscles of the abdominal wall. If looked for in these cases tenderness at the origins and the insertions of the muscles can sometimes be found.
In cases of spinal pain in which muscle spasm is obvious it is also obvious that the muscle spasm is not a source of pain. In an acute attack or acute exacerbation of low back pain the muscle spasm is not only palpable but often visible, running from the sacrum up to the level of the mid-scapulae. Neither the patient nor the examiner can attribute either pain or tenderness to this protective muscle spasm. Sometimes one can find a small localized bundle of painful and tender muscle cramping, particularly in the supraspinatus and gluteal muscles, which may be due to local anoxia, due in turn to localized contraction of an arteriole - itself a reaction to pressure of the spastic muscle. Sometimes one can palpate tender areas at the origins or insertions of the spastic muscles which are, no doubt, due to the long continued hard pull on these structures.
The Swedish orthopaedic surgeons believe that "periarticular fibrositis" of the shoulder and "epicondylitis" at the elbow are effects of the "cervical disc lesion syndrome". The explanation is probably that the limitation of motion by the spasm of muscles about the shoulder, continued over a long period, results in the laying down of adhesions around the Joint, which may proceed to a frozen shoulder. Calcification about the insertion of the supraspinatus tendon also may result from the continuous involuntary spasm which, to a great extent, immobilizes the muscle and almost completely immobilizes its tendon, as calcium tends to be laid down in inactive tissue. The long continued spasm of the extensor muscles of the forearm causes the pain around the radio-humeral joint.
THE "HERNIATED DISC"
The intervertebral disc does not herniate. Herniation of the fibrous nucleus into the spinal canal does occur of course, but in such a small proportion of cases that to apply the term to the whole syndrome is unsound practice, and leads -to a great deal of futile physical, laboratory and radiological investigations. Also it is usually impossible to say definitely whether the nucleus has herniated or not before examination at operation.
The "herniated disc" was first described by Kocher in 189620 and was later described by Middleton and Teacher (1911)21 and again by Mixter and Barr (1934 )22 . Kocher, and Middleton and Teacher described cases in which the patients had suffered severe injuries and the diagnosis was made at autopsy. Mixter and Barr connected sciatica with herniated discs and laid the foundation for the modern concept. This was a great contribution to surgery, but in all other respects the emphasis on the herniation and the surgical aspects of disc lesions have, with the passage of time, proved to be unfortunate.
HERNIATION OF THE NUCLEUS INTO THE SPINAL CANAL IS NOT THE CAUSE OF SPINAL PAIN
The herniation may increase the pain, if the fibrous nucleus, oozing through the annulus, begins to irritate the anterior dura and the adjacent dural sleeve. At this stage a fall may jolt the nuclear mass into the spinal canal which was what probably happened in the cases described by Kocher, and Middleton and Teacher.
The herniation will lessen the pain if a large part of the nucleus escapes the clutches of the posterior lamellae and thus irritates only the dura and the dural sleeve.
If the nucleus slides laterally so that it loses contact with the annulus, the dura, and the dural sheath of the root, pain disappears altogether. A case in point is a patient who was a candidate for operation. Clinically and by myelogram it seemed clear that he had an actual herniation of the nucleus into the left side of the spinal canal. Before he was admitted to hospital he was in a car accident. He was thrown out of the car and landed heavily on the road on his left side. His injuries were superficial but to his surprise, when he arose his spinal and radiating pains had all gone. Our conclusion was that the heavy fall had jolted the' herniated nucleus laterally so that there was no further contact between it and any of the sensitive structures in the spinal canal. The nucleus must have become anchored in its new position by adhesions, because three years later he had no return of symptoms.
"MASSIVE HERNIATION" OF AN INTERVERTEBRAL DISC DOES NOT OCCUR
"Massive herniation" has been described but simply does not occur. By the time the nucleus has eroded through the annulus it has been reduced, at most, to about the size and shape of half a peanut. Further, it does not burst into the spinal canal as has been suggested. It insinuates itself, as a result of flexion-rotation movements of the spine. However, in front of the dura in the spinal canal there are many thin-walled veins. At operation, no matter how gently it is attempted, it is not possible to retract the dura without rupturing some of these delicate vessels. When every effort is made to inflict only the minimum of injury and all that is done is the removal of the fibrous nucleus - herniated or not - the amount of blood suctioned out still averages about 300cc. It is a reasonable conclusion that the rare case of "massive herniation" is the result of an injury which forcefully flexes the spine of a person who has an extensively eroded posterior annulus. If sudden violent flexion causes even a small distraction of the posterior parts of the two vertebral bodies it will tear some of these delicate vessels. The "massive herniation" is therefore a haemorrhage.
The bladder and rectal disturbances only occasionally seen in nuclear lesions of intervertebral discs, are, we believe, also the results of haemorrhage. The involved nerve supply is S 2,3,and 4 and it is necessary for the nerve supply on both sides to be damaged to cause demonstrable disturbance'. This is beyond possibility for a herniated nucleus alone.
PRESSURE ON A NERVE ROOT IS NOT THE CAUSE OF RADIATING PAIN
"Sciatica" is the best known example of the radiating pains of nuclear lesions. It has been incorrectly attributed to pressure on nerve roots in the spinal canal by herniated discs. The objections to this idea are overwhelming. We know from surgical experience that the nerve root is hardly ever involved (if possible we remove the nucleus long before it herniates into the spinal canal) and that the reaction of a peripheral nerve to pressure is not what the sufferer from a nuclear lesion describes. When paralysis is present one can observe that the painless motor and sensory paralysis attributable to compression of a nerve root bears little relation to the distribution of the radiating pain from which the patient is also suffering. These two factors must be separated from each other. The radiating pain in a low lumbar nuclear lesion is frequently from the spine into the gluteal muscles, into the muscles of the back of the thigh and down the calf muscles into the dorsum or sole of the foot, with pain or paraesthesiae in several or all the toes. No spinal nerve or likely combination of nerves could produce this pain. Hirsch24 remarked, "To attempt to ascribe the symptoms to a particular nerve root is wishful thinking." It is for this reason that Swedish orthopaedic surgeons use the noncommittal terms "pseudo-sciatica" and "brachialgia". They do not refer to "root pain" or "root signs".
It is a commonplace experience, for example, that sitting on the top rail of a wooden fence causes paralysis of the sciatic nerve from that level down. The paralysis is entirely painless and one is unaware that it has occurred until one moves to get off the fence. The recovery from the paralysis is not accompanied by any pain or even discomfort. A similar common experience is to sit with the legs crossed and to find on arising that the foot has "gone to sleep", or to awaken in the morning with one hand as numb as a plank. Again there is no pain whatsoever in the onset or recovery from the paralysis. Most doctors have seen the common peroneal nerve paralysis from cast compression. This too is completely painless. The burning pain at the point of skin pressure is irrelevant.
Inman and Saunders25 have observed that "a common conception is that sciatic pain is caused solely by pressure on the nerve root. Such a conception cannot be correlated with any of the existing experimental evidence on the effects of nerve pressure."
To achieve compression of a nerve root between one unstable soft tissue and another - the herniating or herniated nucleus and the fluid-filled dural tube - rather unlikely conditions must be met. The erosion of the annulus must have taken place in a direction that put the bulging annulus and the herniating fibrous nucleus immediately in front of the nerve root. The nerve at the level of the intervertebral disc is quite loose and easily slips off the bulge. In order to be compressed the nerve must be held in some way, possibly by a piece of eroded annulus; or by a favourably placed notch in the nucleus; or by the formation of adhesions between the nucleus and the dural tube as the nucleus slowly works its way into the spinal canal. In this last instance the nerve root (it is inside the dural sleeve) is still capable of making excursions from side to side over the bulge.
If the nerve root is held between the fibrous nucleus and the dural tube for only a 'matter of minutes paralysis attributable to that root may be demonstrated, but if it slips off, the paralysis recovers shortly thereafter. Hence, stable paralysis attributable to compression of a nerve root is quite uncommon and the great majority of patients for whom surgery is indicated due to continuing pain and disability have no signs of sensory or motor paralysis.
Falconer26 in animal experiments, placed wax blocks under nerve roots at the levels of the lumbar intervertebral discs. Immediately after the animal's recovery from the anaesthetic, paralysis attributable to that root was observed, but in about forty-eight hours the paralysis had completely recovered, indicating that the nerve root had adapted by stretching. On re-examination of the animal it was. found that the wax block was still in place. Therefore stretching alone is not enough, the nerve must be compressed continuously.
One investigator placed nylon threads around the nerve roots, brought them to the surface and closed the wound. He observed that pulling on the threads caused pain and regarded this as proof that pressure on the root was the cause of pain. But, the traction he applied was a considerable stimulus to the nervus sinu vertebralis on that side, so he might have been causing the same momentary pain that is caused by movement of the root by a retractor. The exact type and distribution of the pain were not described.
Many patients complain of pain which for some weeks runs down one leg and which then moves and runs down the other leg, and a few patients have an almost equal radiation down both legs. This cannot be explained by nerve root irritation or compression, but is easily explained by the movement of the fibrous nucleus inside an extensively eroded posterior annulus.
One occasionally sees patients who, in addition to their low back pain and sciatica, suffer from a momentary stab of pain and twitch of muscle fibres from time to time. It is probably due to a nerve root being flicked by the bulging annulus, or herniating nucleus, in response to spinal movement.
Inman and Saunders wrote that "The patient often gives a history of numbness in the part. Nevertheless the physician on examination of skin sensation is unable to discern anything of an objective nature, except perhaps a slight hyperalgesia. There is no diminution of peripheral sensation and no anaesthesia, no hypasthesia, no muscle weakness and no definite reflex changes. A puzzling feature to the physician is the fact that the distribution of the patient's pain is frequently constant in direction and position, yet fails to correspond to the area of any known peripheral nerve or nerve root."27
At operations on intervertebral discs it is usually quite obvious that there has been no interference with the nerve root and that the pain the patient has suffered cannot be attributed to this cause.
Further, in the lumbar spine the nerve roots cross the intervertebral discs almost vertically but as one moves up the spine the inclination approaches the horizontal. In the dorsal spine the nerves cross the vertebral bodies. They have no contact with the annulus and are unlikely to be affected, even by a herniation. In the cervical spine the roots run upwards on the vertebral bodies and it is a matter of even greater difficulty for a herniated nucleus to trap and compress a nerve root. Radiating pain analagous to pseudo-sciatica occurs in both regions.
The following experiment settles the question of radiating pain's being attributable to a nerve root. If an anaesthetic solution is injected via the sacral canal into the spinal canal in the prone patient the solution lies in front of the dura and between it and the anterior surface of the spinal canal. This has been demonstrated in x-rays by the use of a contrast medium".
The anaesthetic solution runs up to the level of about the 3rd lumbar vertebral body. The patient's low back pain and the radiating pain running down the leg is completely relieved but there is no paralysis. We have done this experiment using an anaesthetic solution as weak as .04% which has practically no effect on the large nerve roots but anaesthetize the minute unmyelinated threads of the nervi sinu vertebrales. We have used stronger anaesthetic solutions in sacral extra-dural injections several thousand times. Complete relief of the low back pain and the radiating pain is secured without paralysis in the legs. Saddle anaesthesia results when the stronger solutions are used, but most patients hardly seem to be aware of it. The relief of pain from these injections is proof that the nerve roots are not a factor in radiating pain.
And finally, at the risk of being drearily repetitive, we must say again that pressure on peripheral nerves causes painless paralysis.
One may speculate on the reason why comparatively light pressure on a nerve causes arrest of function. It may be that fluid is pressed out of the part of the nerve being compressed and that a comparatively dehydrated nerve cannot transmit electric current. The motor fibres, being the largest, are most easily affected. The smaller sensory fibres need a greater pressure to cause arrest of function and the minute pain fibres remain unaffected.